New Resource: HCC Tearsheet 2025. Access Now!
New Resource: HCC Tearsheet 2025. Access Now!
Our analytics technology allows you to prioritize interventions for the patients that need it the most.
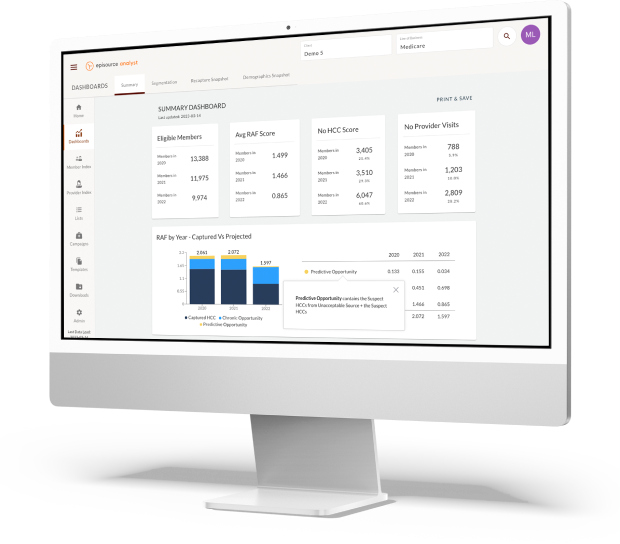
Episource Analyst is an essential tool for Medicare Advantage and Medicaid provider organizations in risk-based agreements. Its advanced analytics and recommendations can be used to accurately assess the health risks of your patient population.
More importantly, this information can also be used to execute earlier interventions for your patients. Find all the analytics you need quickly and efficiently.

Generate chase lists by prioritizing high-risk members for more immediate care.
Customize your member- and provider-level reports and easily view campaign performance metrics, such as total eligible members and top five suspected and captured HCCs with our intuitive UI.
Drive primary and specialty care by analyzing gaps
Support case management for high-risk members
Strengthen your prospective care strategy
Drive primary and specialty care
Make data-driven decisions with robust reporting features
Drastically reduce workflow inefficiencies
They’ve added in features where we can actually see the campaigns in real time and watch it progress through the dashboards and get all kinds of great reporting.
Seamlessly Transition to the V28 Model with Episource Analyst
In early 2023, the Centers for Medicare & Medicaid Services (CMS) announced the transition to Version 28 of the CMS-HCC model. The V28 model is expected to decrease Medicare Advantage risk scores by an average of 3.56% in 2024. Episource Analyst can help you plan ahead with:
Our analytics technology ingests your member data to estimate the potential decrease in risk scores and RAF opportunities for your risk adjustment program.
We’ll provide you with a more accurate risk assessment of your member population based on the changes to unique HCCs and HCC mapping.
Our experts will share strategies for counteracting a decline in risk scores, such as developing prospective care programs and improving member engagement.
